Abstract
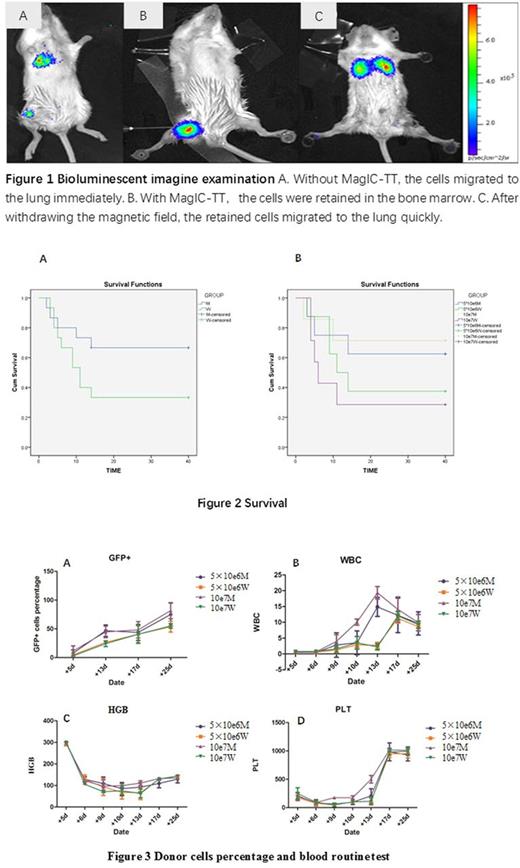
Background: Intra-bone marrow transplantation has been proven to be efficient in improving the homing of transplanted cells, resulting in faster hematopoietic reconstitution and a reduction in severity of GVHD. However, because of staggered blood vessels in bone, many transplanted cells leak out to peripheral circulation. In our previous study (Blood 2015 126:5404), it has been initially proven that MagIC-TT could enhance target transplantation to femurs by flow cytometry and pathological examination. After that, by bioluminescent imagine system, we further proved that most intra-bone marrow transplanted cells moved to lung immediately without MagIC-TT (Figure 1 A); while the cells were retained in the bone marrow with MagIC-TT (Figure 1 B), but if the magnetic field withdrawal 1 hour after, the cells also moved to the lung quickly(Figure 1 C). In this study, the therapeutic effect of intra-bone marrow transplantation combined with MagIC-TT was explored in allogenic murine transplantation model.
Methods
Mice and cell preparation: Sixty female BALB/c mice with specific pathogen free (SPF) were randomly separated in 4 groups (16 and 14 mice in 5×10e6M and 1×10e7 M group respectively; 16 and 14 mice in 5×10e6W and 1×10e7 W group respectively, M/W referring to MagIC-TT/non-MagIC-TT). The recipients received 7.5Gy irradiation before transplantation. Twelve SPF C57BL/6 CAG-eGFP transgenic mice were used as donors. The bone marrow were magnetized by nanoparticles and then adjusted to the concentration of 5×10e6/20μL and 1×10e7/20μl for use. Every mouse was injected with 20μL, 5×10e6 or 1×10e7 cells.
Intra-bone marrow injection and fixed magnetic field After anesthetizing the mice and disinfecting the knee joint, the femoral puncture was operated with the medulla-puncture needle invented by our team (Chinese patent No.201620090904.2). In M groups, special magnetic fields were applied to the femurs of mice during and after injection. The effects of intra-bone marrow injection had been proven by X-ray and bioluminescent imaging system, etc .
The therapeutic effects The therapeutic effects were determined by the survival of mice, the percentage of GFP+ cells in peripheral blood, blood routine test etc. to evaluate the hematopoietic reconstitution.
Results
Survival: The survival rate was 66.7% and 33.3% in M groups and W groups on the 40th day after transplantation (P=0.096) (Figure 2 A), which was 62.5% and 71.4% in 5×10e6M and 1×10e7M, 37.5% and 28.6% in 5×10e6W and 1×10e7W, respectively(Figure 2 B).
Donor cells percentage in peripheral blood (Figure 3 A): Flow cytometry analysis was performed on the 5th, 13rd, 17th, and 25thday after transplantation. The percentage of donor GFP+ cells grew much faster on d5~d13 in M groups than that in W groups (P<0.05). Pairwise comparisons showed that 10e7M group grew faster than 10e7W (P<0.05), donor GFP+ cells in 5×10e6M grew even faster than those in both 5×10e6W and 1×10e7W (P<0.05). No significant difference was found between 5×10e6M and 1×10e7M.
Blood Routine Test: Generally, WBC in M groups reached growth peak on d9-13 vs d13-17 in W groups, and the WBC number of M groups are higher than those in W group (P<0.05) (Figure 3B). This trend also existed for HGB and PLT, but not as significant as WBC (Figure 3 C, 3 D) .
Conclusion
MagIC-TT can improve the effect of intra-bone marrow transplantation by avoiding transplanted cells leakage to peripheral circulation, resulting in faster hematopoietic reconstitution in allo-murine transplantation model. The mechanism of MagIC-TT and its relation with reduction of complication are under further study.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal